Epidemiology is the method used to study health outcomes and the frequency of diseases in different groups of people. It’s crucial for researchers to understand the epidemiology, and especially the distribution, of amyotrophic lateral sclerosis (ALS) throughout micro and macro populations.
Understanding epidemiological factors and collecting real-world data allow scientists worldwide to share information, compare and contrast risk factors in different populations, and collaborate on treatments. Collecting this valuable information can also help patients and families learn about the current statistics regarding incidence, treatments, and outcomes and build a deeper understanding of their options.
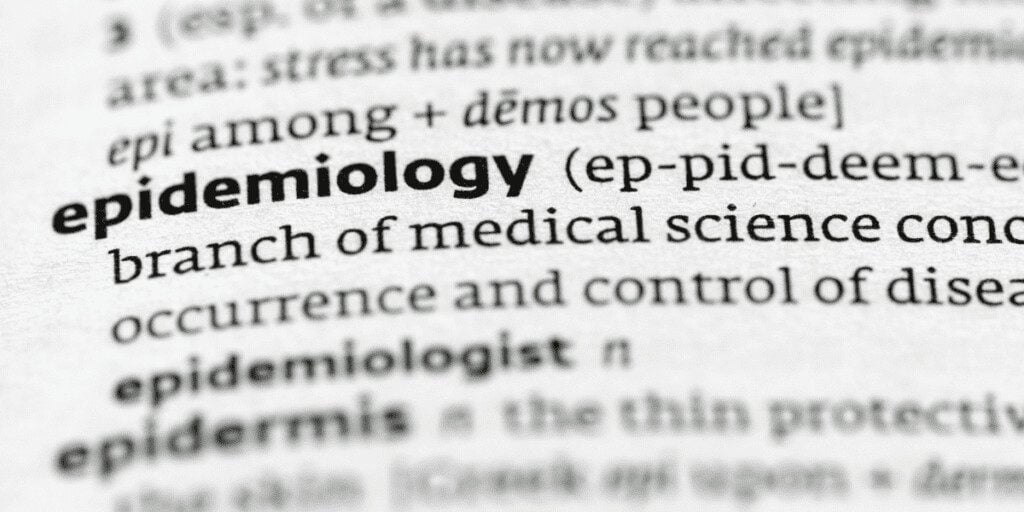
While it’s a rare disease, ALS can significantly impact patients’ (and their families) lives. When researchers pay close attention to epidemiological factors of ALS and study the incidence and prevalence of the disease and any disease clusters, they gain critical insight into social, political, environmental, and economic factors among people of different ages, sexes, ethnicities, locations, and socioeconomic backgrounds.
What is the ALS Incidence Rate?
When describing ALS cases in the U.S. and worldwide, it’s essential to understand the difference between incidence and prevalence. While they may seem similar, incidence refers to the proportion of people who develop a disease during a specific time period (in other words, new cases) and prevalence includes all cases in the population at the specified time period.
A study published in 2022 found that the age-adjusted incidence rate for ALS went from 1.7 to 1.5 per 100,000 people in the U.S. from 2014 to 2016.1 However, the cases were compiled using data from the Centers for Medicare and Medicaid Services, the Veterans Health Administration, and the Veterans Benefits Administration, along with volunteers of all ages who were counted voluntarily using a secure registry.2 In 2015, the CDC reported that the annual incidence was about 2 per 100,000 people in the U.S.3
In Europe, ALS incidence rates are higher. They hover around 2.6 per 100,000 in European ALS registries.4 However, countries like Stockholm and Scotland saw ALS incidence of 3.8 per 100 000 prior to 2017.5
It’s important to note that methodological differences in collecting data can contribute to differences in incidence rate reports.6 The populations measured, the completeness of the data, the timing of the data collection, and the definition of a diagnosis can all affect these numbers.
Is the Incidence of ALS Increasing?
One of the only studies to date that has attempted to estimate the number and distribution of future ALS cases predicted that the worldwide annual incidence of ALS would increase by 69% in the next 25 years.7 The authors estimate the current worldwide ALS incidence to be 1.9 per 100,000.
If the projection is correct, the total number of worldwide ALS cases will increase from 222,801 in 2015 to 376,674 in 2040. An essential part of this estimate is the increasingly aging population. ALS tends to be diagnosed in people over age 60.
By understanding the epidemiology of ALS and the potential for a significant increase in ALS incidence rates, many researchers hope that healthcare experts and policymakers will dedicate more resources to understanding the disease.
What Percentage of the Population has ALS?
Prevalence refers to the number of cases (both new and existing) of a disease in a specific population at either a particular point in time or over a specified period.8 Because it’s a rare disease, ALS prevalence is calculated as cases per 100,000 rather than as a percentage.
The prevalence of a disease is typically reported as a percentage or as the number of cases per 10,000 or 100,000 people.9 For example, according to the CDC, ALS prevalence is roughly 4 to 6 per 100,000 people.10
However, the National ALS Registry, which collects data on ALS patients in the U.S., reported an ALS prevalence rate of between 5.0 and 5.2 per 100,000 people in 2014- 2016. Correcting for undercounting errors and a lack of available data, researchers have recently adjusted these rates to over 7 cases per 100,000 people. They believe an upper-bound estimate may be closer to 9.9 per 100,000 people in the U.S.11
Is ALS More Prevalent in Men or Women?
Data from the Center for Disease Control suggests that ALS is slightly more prevalent in men than women, especially at a younger age. Men also have a slightly higher incidence rate than women. As people age, the risk of developing ALS tends to even out between sexes.12
ALS also tends to affect caucasian people more often than other demographic groups and is more common in those ages 60–69 years. However, ALS can occur in people of all ethnicities and all ages. Most cases (90 – 95%) also occur sporadically – that is, in those with no familial history of the disease.
The data shows that non-Hispanic white men over 60 are technically at higher risk for the disease, even though it is rare. But this may also result from having access to a system that can render a diagnosis. Data on the prevalence of ALS among minority groups and others who receive less biomedical healthcare is bound to be sparse.
What are the Most Common Risk Factors Among ALS Patients?
Risk factors for ALS appear to include sex (it is more common in men in those diagnosed before age 70) and age (ALS is most commonly diagnosed between the ages of 40 and 65). This is especially the case in sporadic ALS cases. Heredity is also an ALS risk factor. Even though only 5 to 10% of people with ALS have a familial (inherited) version, they are more likely to pass on a genetic mutation associated with ALS to their children. In those with early-onset familial ALS (fALS) , their offspring appear to have a 50% chance of developing the disease themselves. Environmental factors such as cigarette smoking have also been linked to an increased risk of developing ALS. Smoking at a young age has also been associated with a higher risk of ALS.13 The CDC’s National ALS Registry not only records the incidence, prevalence, and demographics of people with ALS, but it also attempts to examine environmental and occupational risk factors. However, just because there is a correlation between an environmental factor and ALS does not mean there’s a causal link. Therefore, these risk factors (such as exposure to heavy metals and pesticides) require more investigation.

The Power of Data for Understanding ALS
Just like the collaborative platforms for ALS research and tissue analysis that Target ALS provides, ALS registries bring together details of ALS cases so that we can understand how many people have the disease and at what rate it affects some groups more than others.
Epidemiological studies are complex and take enormous amounts of data to produce. In fact, when more data is added, our picture of the incidence, prevalence, and risk factors can change. This is one of the reasons organizations like Target ALS are working on compiling as much data as possible on people with ALS worldwide.
Frequently Asked Questions:
What is epidemiology?
Epidemiology refers to the incidence rate and distribution of disease and any patterns and other factors that affect causes and risk factors in specific populations.14
Are there any known clusters of ALS?
While it appears to be significant when multiple people in a community are diagnosed with ALS, this is sometimes due to better diagnostics or the presence of a specialized medical center or its staff in that same community. In this case, the cluster would not be due to an environmental factor. We can’t say that having someone knowledgeable about ALS in a community is more likely to cause the disease – they are simply more likely to reveal it.
While clusters have been identified around the world (from France to Chile to New Hampshire), none have revealed anything about a specific environmental source of the disease. Only one cluster in the western Pacific islands (Guam) is suspected to be notable, and the population no longer appears to be at an elevated risk.15
Where are most cases of ALS?
In the U.S., the Midwest currently has the largest number of people with ALS (at 5.5 cases per 100,000 population).16 Researchers have also found that the prevalence rates of ALS are highest in Uruguay, New Zealand, and the United States.17
How common is ALS worldwide?
Global estimates of ALS range from 1.9 per 100,000 to 6 per 100,000.
Who is most at risk for ALS?
Current data indicates that ALS is more common in white men between the ages of 60 – 79. However, anyone of any age can get ALS, and we haven’t yet identified all the risk factors.
Sources:
1. Mehta, P. et al. (13 Jan 2022). Incidence of amyotrophic lateral sclerosis in the United States, 2014–2016. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. https://www.tandfonline.com/doi/full/10.1080/21678421.2021.2023190
2. Mehta et al., 2022.
3. Centers for Disease Control. (23 Nov 2018). Prevalence of Amyotrophic Lateral Sclerosis — United States, 2015. Morbidity and Mortality Weekly Report. https://www.cdc.gov/mmwr/volumes/67/wr/mm6746a1.htm
4. Mehta et al., 2022.
5. Longinetti, E. and Fang, F. (12 Aug 2019). Epidemiology of amyotrophic lateral sclerosis: an update of recent literature. Current Opinion in Neurology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6735526/
6. What is prevalence? National Institute of Health. Retrieved on October 31, 2022, from https://www.nimh.nih.gov/health/statistics/what-is-prevalence
7. Arthur, K. et al. (11 Aug 2016). Projected increase in amyotrophic lateral sclerosis from 2015 to 2040. Nature Communications. https://www.nature.com/articles/ncomms12408?origin=ppub
8. Prevalence vs. Incidence: what is the difference? Cochrane Collaboration. (6 Nov 2020). Retrieved from https://s4be.cochrane.org/blog/2020/11/06/prevalence-vs-incidence-what-is-the-difference/
9. What is prevalence? National Institute of Health. Retrieved on October 31, 2022, from https://www.nimh.nih.gov/health/statistics/what-is-prevalence
10. Centers for Disease Control, 2018.
11. Mehta, et al., 2022.
12. What is Amyotrophic Lateral Sclerosis? Centers for Disease Control. (13 May 2022). Retrieved from
https://www.cdc.gov/als/WhatisAmyotrophiclateralsclerosis.html
13. Wang, H. et al. Smoking and Risk of Amyotrophic Lateral Sclerosis: A Pooled Analysis of 5 Prospective Cohorts. JAMA Neurology. (Feb 2011). https://jamanetwork.com/journals/jamaneurology/fullarticle/802279
14. What is epidemiology? Centers for Disease Control. (17 Jun 2016). Retrieved from https://www.cdc.gov/careerpaths/
15. Spencer, PS. et al. (Dec 2019). ALS and environment: Clues from spatial clustering? Revue Neurologique. https://www.sciencedirect.com/science/article/abs/pii/S0035378719306046
16. Centers for Disease Control, 2018.
17. Arthur, K. et al., 2016.