What is ALS?
Amyotrophic lateral sclerosis (ALS) is a progressive, incurable neurodegenerative disease that leads to the irreversible degeneration of motor neurons. Motor neurons are the nerve cells in the spinal cord and brain that initiate and control muscle movement.
Only about 2 out of every 100,000 people will get the disease each year, and it typically affects those between ages 40 and 70. More than 90% of ALS cases are sporadic (no clear family history), and 5% to 10% of ALS cases are familial (inherited through a mutated gene).1 Typically, the disease will progress over 2 to 5 years after diagnosis. However, 20% of patients live for more than 5 years, and about 5% live for 20 years or more.2
The name describes the condition. Amyotrophic comes from the Greek. A means “no,” myo refers to “muscle,” and trophic means “nourishment.” Lateral refers to the areas in the spinal cord where portions of the nerve cells that signal and control the muscles are located. As this area degenerates, it leads to scarring or hardening, known as sclerosis.
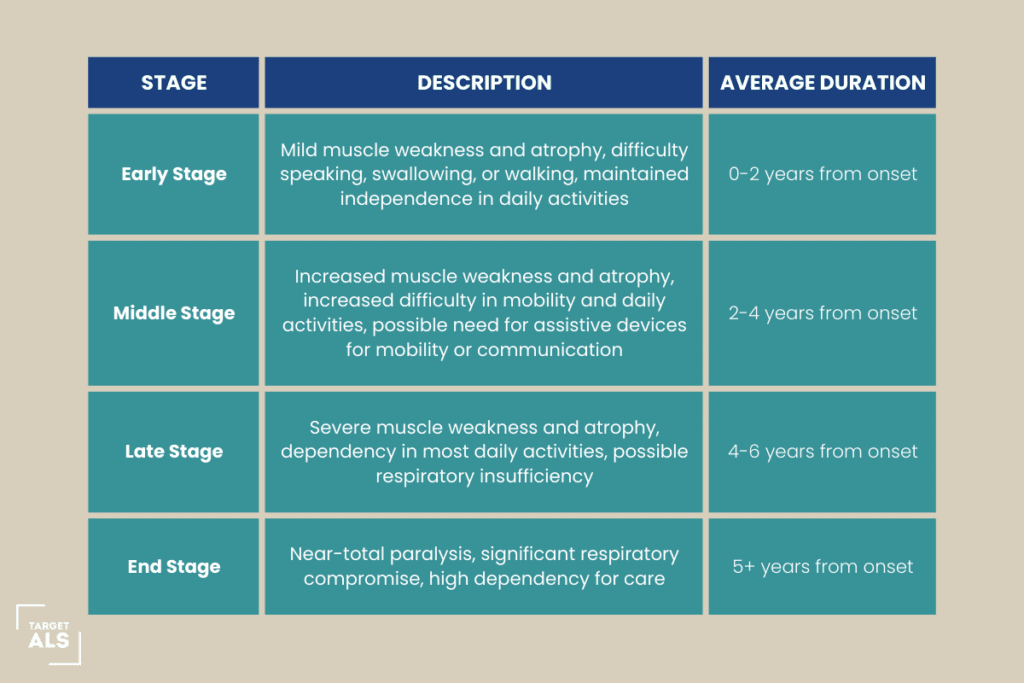
How quickly does ALS progress?
It varies. It does not progress linearly: There is no “ALS timeline.” As the disease advances, muscle weakness and atrophy spread, leading to difficulties with moving, speaking or forming words (dysarthria), breathing (dyspnea) and swallowing (dysphagia). Dysphagia makes it difficult to eat. At the same time, people with ALS burn calories at a faster rate than average. As a result, they lose weight rapidly and become malnourished.3
Because ALS disease progression varies by the individual, precise staging is tricky. That’s one reason the reason many clinicians — at least when dealing with patients and caregivers — will frame ALS progression in terms of three broad categories: early, middle and late. Some will add a fourth, termed the “end” or “final” stage.
Generally speaking, ALS is a progressive illness which means it gets worse over time.
Early-stage ALS
The first signs of ALS often occur long before diagnosis. It initially manifests one of two ways: as weakness in the limbs, called limb (or spinal) onset, or difficulty in speaking or swallowing, termed bulbar onset.4 Limb onset is far more common.5
Early symptoms can include muscle weakness, spasticity (tightness), cramping, and/or fasciculations (twitching). Because this frequently begins in the arms or hands, it makes daily tasks challenging. Symptoms typically start in one region of the body, although mild symptoms may affect other areas. The person may feel fatigued, have poor balance, have a weak grip or stumble when walking.
Bulbar-onset ALS begins in the face or neck. Early symptoms include slurred speech and hoarseness. The person may be experiencing ALS throat symptoms like difficulty chewing and swallowing — aspirating or choking while eating.6,7
Diagnosis stage of ALS
The diagnosis stage of amyotrophic lateral sclerosis (ALS) entails a thorough examination by medical personnel to determine the disease’s presence. Diagnosis of ALS can be difficult because there is no single test or clear marker for the disease. To make an accurate diagnosis, healthcare personnel rely on a mix of clinical examinations, medical history analysis, and the exclusion of other probable reasons. While difficult, this stage is critical because it lays the groundwork for effective management and assistance.
Numerous examinations and investigations are frequently carried out to rule out other illnesses that can resemble the symptoms of ALS. These could include blood tests to measure particular biomarkers and rule out alternative diagnoses, nerve conduction studies (NCS) to gauge the strength and speed of nerve signals, electromyography (EMG) to gauge muscle electrical activity, and imaging methods like magnetic resonance imaging (MRI) to view the brain and spinal cord.
Middle-stage ALS
How fast does ALS progress after the first symptoms? In the middle stage of ALS, the early-stage symptoms become worse. Muscle atrophy will spread to other parts of the body, increasing weakness. Some muscles become paralyzed, and some may become shortened, preventing joints from fully straightening.8
Overall weakness increases and walking becomes more challenging. If the person falls, they may not be able to get back up on their own. Driving is no longer an option, and the individual may need help with the activities of daily living.
Swallowing and chewing may become increasingly difficult over time, and the risk of choking increases. Breathing also becomes harder.
Some people experience uncontrollable bouts of laughing, called the pseudobulbar affect. These happen completely randomly and aren’t related to outside stimuli.
Middle-stage ALS: The 2nd Region
As the second region of engagement intensifies, people may have breathing difficulties. As breathing muscles like the diaphragm and intercostal muscles deteriorate, lung capacity and breathing effectiveness decline. Breathing difficulties, exhaustion, and an increased risk of respiratory infections may result from this. To help with breathing and increase survival, respiratory support alternatives like non-invasive ventilation or eventually invasive ventilation may be taken into consideration.
In addition to physical changes, the middle stage of ALS often brings emotional and psychological adjustments. The progressive loss of independence and the need for increased assistance can lead to feelings of frustration, sadness, and a sense of loss. It is crucial for individuals with ALS to have access to a supportive network of healthcare professionals, caregivers, and support groups to address their emotional well-being and provide guidance during this challenging stage.
Middle-stage ALS: The 3rd Region
The disease spreads to the third region, which predominantly consists of the trunk and core muscles, in the intermediate stage of amyotrophic lateral sclerosis (ALS). A person’s mobility, stability, and capacity to keep an upright posture are all impacted by this process in further detail.
The muscle weakness and atrophy that first afflicted the bulbar region, then moved to the arms and legs, now affects the trunk as ALS progresses. It becomes harder to maintain balance, stability, and core strength when the muscles surrounding the pelvic, back, and abdomen lose strength and coordination with time.
Mandatory gastrostomy stage ALS
People with amyotrophic lateral sclerosis (ALS) may progress to the point where they must have a gastrostomy. In this stage, a feeding tube is placed directly into the stomach to deliver enough nourishment and fluids when swallowing becomes seriously compromised.
Late-stage ALS
In advanced ALS, most voluntary muscles are paralyzed, including those of the mouth and throat. So are those involved in breathing. Poor respiration can lead to fatigue, headaches and impaired thinking.9 It also increases their susceptibility to pneumonia. Ultimately, they may need to rely on a ventilator. Mobility is extremely limited. Talking and swallowing become more difficult. That makes eating exceptionally difficult, and the individual eventually will require a feeding tube.
Final stages of ALS
ALS is always fatal, and most deaths result from respiratory failure. Medications can relieve discomfort, anxiety and fear caused by respiratory insufficiency.
Hospice care helps ensure the person with ALS has the most peaceful, dignified and painless experience possible. In general, patients with a prognosis of six months or less are considered eligible for hospice, but that varies. Only a physician can make a prognosis, but these signs suggest that the person may be ready for hospice:10
- Speech has become barely intelligible, unintelligible or impossible.
- The person with ALS needs considerable assistance with — or is totally dependent on others for — eating, dressing and grooming.
- The patient does not wish to be dependent on feeding tubes for nutrition and hydration
- The patient does not want to be placed on a ventilator or wishes to discontinue mechanical ventilation
Hospice care can control pain and help manage symptoms while providing emotional and spiritual support for the person with ALS and their family. In addition, patients using hospice care are more likely to stay in their preferred location, die outside the hospital and receive appropriate pain management.11
How long does the final stage of ALS last?
The final stage of ALS varies quite a bit from person to person. During this phase, patients typically experience significant muscle weakness, respiratory challenges, and require extensive support for daily activities.
The duration of this last stage can range anywhere from several months to a few years. It’s influenced by several factors including respiratory health, overall well-being, nutritional status, the level of medical and palliative care received, and personal treatment decisions made by the patient and their family.
Turning to more precise staging
Framing ALS disease progression based on these four simple stages makes sense for helping patients and families understand what lies ahead. But for researchers and many physicians, it’s inadequate. Staging ALS is imprecise. The very nature of the disease means that there will never be a perfect way to measure progression, but researchers need more exact staging tools.
One, the Milano-Torino staging system (MiToS), is based on functional ability. It focuses on a number of functional domains with a loss of independent function: movement (which includes walking and self-care), swallowing, communicating and breathing.12
Another, more common, approach is the King’s ALS clinical staging system. It assesses anatomical spread of ALS based on the number of affected regions (bulbar, upper limb and lower limb). It also includes advanced stages defined by nutritional or respiratory failure.13 Scores range from Stage 1 for early disease with one region involved, to Stage 4, for late disease:
ALS Symptom Progression Timeline
- Stage 1: Symptom onset (involvement of first region)
- Stage 2A: Diagnosis (35% of the way through the disease course)
- Stage 2B: Involvement of second region (38%)
- Stage 3: Involvement of third region (61%)
- Stage 4A: Need for gastrostomy (a feeding tube) (77%)
- Stage 4B: Need for noninvasive ventilation (80%)
A 2020 study found that both systems may effectively assess changes in patients’ clinical progression and treatment responses.14
Why accurate staging matters
Accurate staging is not only essential for clinical trials, but it may also inform how clinicians discuss ALS with patients and caregivers. “The independent and complementary nature of the 2 systems, one tracking anatomical spread of disease (the King’s Clinical Staging System) and the other focusing on loss of function (the MiToS system), means they can provide different insights that may be particularly important in counselling patients on the potential benefits of therapy,” the researchers wrote.14 [1]
Much remains unknown about this disease, and researchers around the world are trying to learn more develop new ALS therapies and diagnostics. To learn about some of these efforts, visit www.targetals.org/research/.
Rare Forms of ALS
Some rare forms of ALS include:
Progressive Muscular Atrophy (PMA)
PMA is another rare variant of ALS that primarily affects the lower motor neurons in the spinal cord. Unlike classic ALS, which affects both upper and lower motor neurons, PMA primarily involves muscle weakness and atrophy without significant spasticity. PMA tends to progress more slowly than typical ALS.
Flail Arm Syndrome (FAS)
These are rare variants of ALS characterized by predominant weakness and atrophy either in the arms (FAS) or legs (FLS), with relative sparing of other muscle groups. These variants often progress more slowly than classic ALS and may have a better prognosis in some cases.
Juvenile ALS
While ALS typically affects individuals over the age of 40, juvenile ALS refers to cases that develop in individuals under the age of 25. Juvenile ALS may have unique genetic or environmental factors contributing to its onset.
ALS Life Expectancy Chart
Frequently Asked Questions
What is limb onset MND?
A limb-onset disease implies that the initial symptoms are in the arms or legs. This could be as subtle as a weakened grip, difficulties lifting or holding onto objects, or even trouble lifting your arms above your head. Many individuals struggle with daily physical actions like walking up stairs.
What is the average life expectancy after ALS diagnosis?
The average life expectancy after ALS diagnosis is about 3 to 5 years. In certain instances, patients can survive for longer than a decade.
How quickly does respiratory onset ALS progress?
ALSFRS is a scoring system used to measure the progression of ALS, from swallowing to breathing and climbing stairs. If the decline is more than half a point every month, respiratory symptoms are worsening faster.
How does foot atrophy manifest itself in ALS?
Foot atrophy in ALS typically manifests as a progressive weakening and wasting away of the muscles in the feet due to the degeneration of motor neurons that control muscle movement.
SOURCES
- Genetic Testing for ALS. ALS Association https://www.als.org/understanding-als/who-gets-als/genetic-testing
- Amyotrophic Lateral Sclerosis (ALS) Fact Sheet National Institute of Neurological Disorders and Stroke
- National Institute of Neurological Disorders and Stroke op. cit.
- https://alsnewstoday.com/forms-of-als/
- https://www.als.net/news/science-sunday-limb-and-bulbar-onset-als/
- https://emedicine.medscape.com/article/1170097-overview
- https://alsnewstoday.com/stages-of-als/
- https://alstreatment.com/als-progression-timeline/
- https://www.vitas.com/care-services/personalized-care-plans-by-diagnosis/als-lou-gehrigs-disease
- https://www.compassus.com/for-caregivers/is-it-the-right-time-for-hospice/end-of-life-care-for-als
- https://alsnewstoday.com/news-posts/2020/12/02/two-als-staging-systems-may-be-useful-assessment-tools-in-clinical-trials-study-suggests/
- Roche JC, Rojas-Garcia R, Scott KM, et al. A proposed staging system for amyotrophic lateral sclerosis. Brain. 2012;135(Pt 3):847-852. doi:10.1093/brain/awr351
- Ibid.
[1] Ibid.