Inside the work of University of Rhode Island researcher, Dr. Riccardo Sirtori
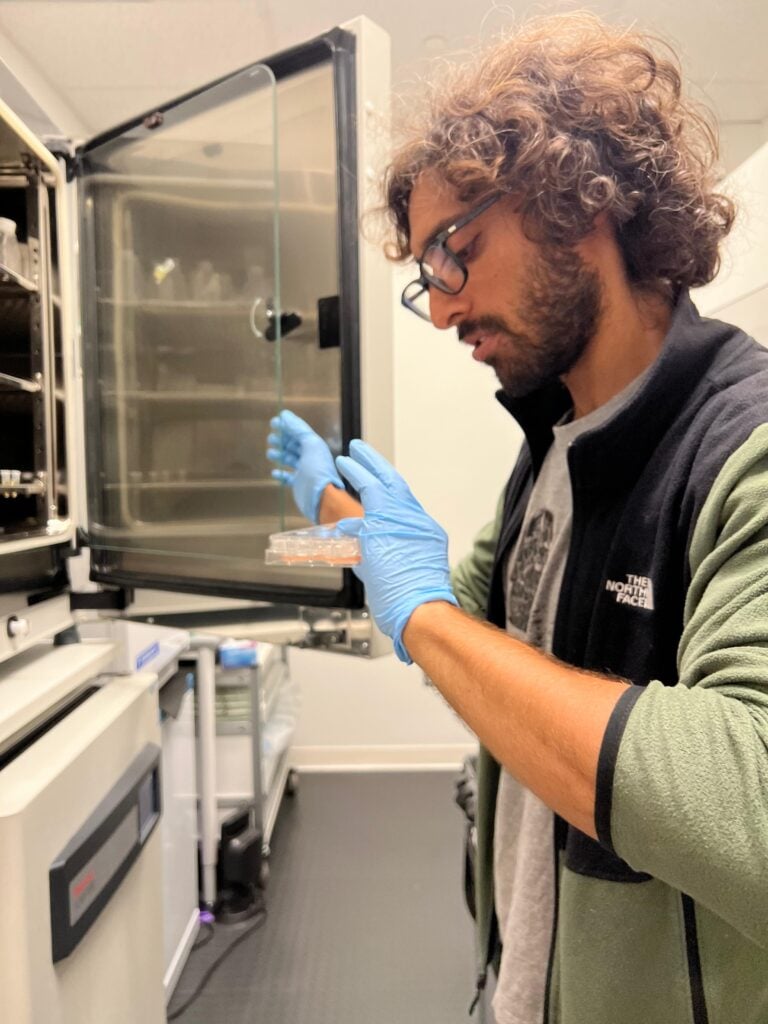
At first glance, the path from medical school in Milan to pioneering biosensor research in Rhode Island may seem unexpected. But for Dr. Riccardo Sirtori, curiosity and collaboration have always been the driving forces behind discovery.
Dr. Sirtori’s interest in biosensing began in 2024 through a collaboration between the neuroscience lab of Dr. Claudia Fallini and the nanosensing lab of Dr. Daniel Roxbury at the University of Rhode Island. Dr. Roxbury, a chemical engineer, is an expert in nanosensing, and Dr. Sirtori was introduced to the technology by a former roommate, Rodrigo Monroy Lopez, who works in the lab. The two fields, engineering and neuroscience, converged in a new way, sparking an idea that could reshape how ALS is diagnosed.
“We started this collaboration mainly because my former roommate was working in this lab, and I got interested in the technology he was using,” Dr. Sitori explained. That technology had already been used to differentiate between types of immune cells, but he saw its potential for a different purpose: detecting the molecular fingerprints of ALS.
What is a biosensor and why does it matter for ALS?
“There are no specific diagnostic biomarkers for ALS,” Dr. Sirtori explained. “A biomarker is any analyte or group of analytes that you can use to track either a physiologic or pathologic condition.”
While several candidate biomarkers are being studied in ALS, he said, most are limited to certain disease phases and don’t consistently reflect clinical progression. His team instead uses what the FDA defines as a ‘multi-component integrated biomarker’: a profile that captures a molecular fingerprint of a sample rather than focusing on one molecule.
“So it’s like taking the fingerprint of a person,” he said. “Maybe some aspects or some features inside this fingerprint are shared across different pathologic conditions. And that’s what we are able to see with our biosensing.”
By integrating this complex data through mathematical modeling, the technology can distinguish ALS samples from healthy ones and potentially go further in the future.
From samples to insights
Using serum samples from 39 participants in the Target ALS Global Natural History Study, about half including individuals with sporadic ALS and half including healthy controls, Dr. Sirtori’s team trained a machine learning model to test their approach. This collaborative effort includes machine learning expert Dr. Nicholas Fisk, who guides the creation of the machine learning model and Brown University’s Dr. Vincent LaBarbera.
“Based on our biosensor, we were able to create a machine learning model able to classify the ALS samples versus the healthy non-neurological control samples with an accuracy of 92%,” he said.
Equally important, the molecular features detected by the biosensors also correlated with how quickly a patient’s disease progressed. “Thanks to Target ALS, we have the clinical scores of these patients in the ALS Functional Rating Scale at different times,” he explained. “We were also able to correlate some of the features detected by our sensor with the progression rate of the disease. And this can be extremely useful for prognostic objectives.”
Challenges and next steps
Dr. Sirtori said one of the main challenges in machine learning–based technology is ensuring that findings are generalizable across diverse patient groups. “We need a big amount of samples so that we can acquire as many fingerprints as we can,” he said. “We want to be able to detect those features that are shared among ALS patients in all this possible variability of fingerprints.”
His team is now working to expand their dataset and make the model more specific. “The next step is also to make it more and more specific,” he said. “Include samples from patients who actually don’t have ALS, but maybe have some closely related diseases, like motor neuropathies or other neurodegenerative diseases.”
The power of collaboration and open science
For Dr. Sirtori, collaboration is not just part of the scientific process, it’s the foundation. “For us, it is fundamental,” he said. “URI is a big school, but as a research institute, it’s not as big as others. We don’t have a hospital we refer to. So for us, it’s fundamental; collaboration between labs, between labs and hospitals, between nonprofit organizations like Target ALS and the academic environment, because we literally live out of this.”
He also highlighted the vital role of organizations like Target ALS in providing biobanks and coordination between institutions, calling such partnerships “precious.” His team is now deepening its collaborations with clinicians at Brown University to grow and refine the model.
Access to high-quality biospecimens and longitudinal clinical data through Target ALS has been instrumental in Dr. Sirtori’s progress. The integration of nanoscale technology with open-science collaboration, he said, is helping turn a promising diagnostic concept into something that could one day transform ALS care.