ALS (amyotrophic lateral sclerosis), is a relentless and fatal neurological disease that causes progressive muscle weakness and paralysis, eventually affecting the ability to speak, eat, move, and even breathe. There are currently no treatments available to effectively slow down or halt the progression of ALS beyond a modest amount, and most people with the disease live only two to five years after diagnosis, making it one of the most devastating conditions to endure.
Bridging the Gap: The Urgent Call for Diversity in ALS Research and Healthcare
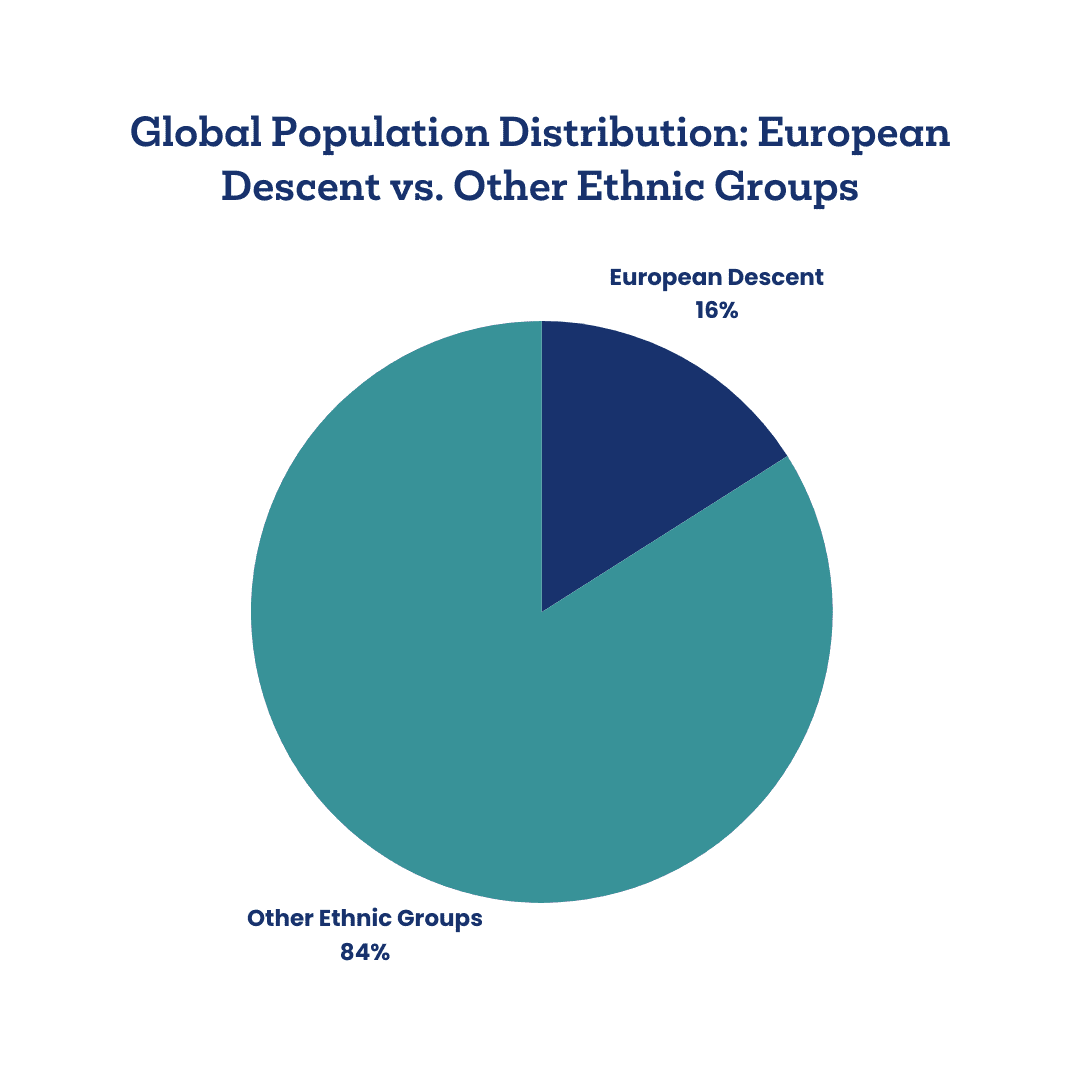
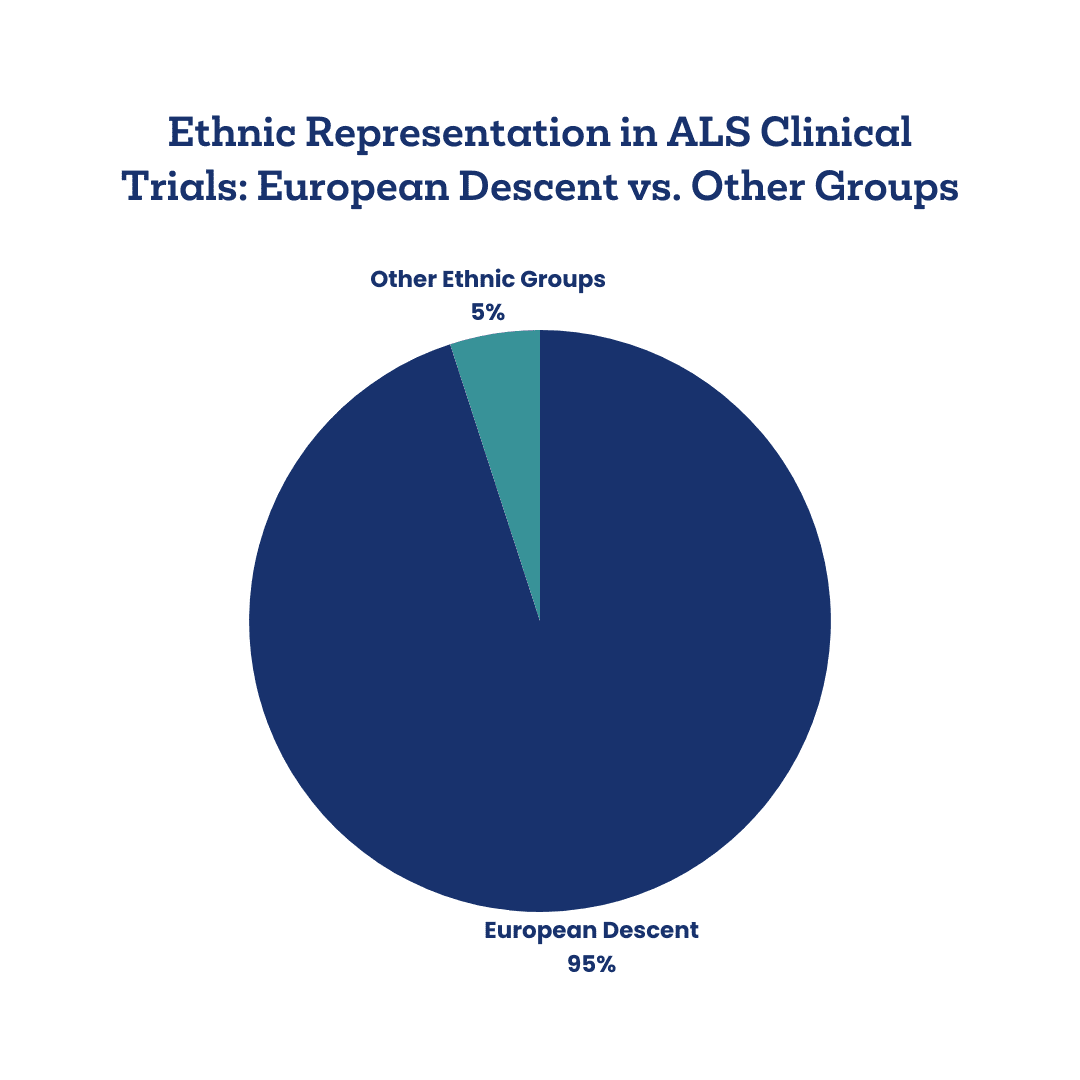
ALS affects individuals across all backgrounds, yet representation in ALS research has long been skewed. Data reveals that approximately 95% of participants in previous ALS clinical trial studies were Caucasian, leaving other populations, particularly Black and Latino communities, significantly underrepresented. This lack of diversity in research critically impacts diagnosis, treatment, and outcomes for underserved groups. Dr. Mita Karra, a neurology resident at UCLA, offers a firsthand perspective on these disparities and shares insights into efforts that Target ALS and others are making to bridge the gap in ALS healthcare for diverse communities.
The Impact of Barriers to Care
“Disparities in accessing healthcare for people with ALS can be due to a multitude of factors, including but not limited to race and ethnicity, age, socioeconomic status, immigration status and availability of health insurance, religion and cultural differences, etc.,” Dr. Karra explains.
Barriers to care contribute to delayed diagnosis, limited access to multidisciplinary care, and missed opportunities for patients to participate in life-extending clinical trials. A recently published review by Perez et al.1, highlights the gravity of these disparities, showing that Black and Latino patients are 30% and 40% less likely, respectively, to consult with an outpatient neurologist for neurological conditions in general. For ALS specifically, Dr. Karra notes, “Black ALS patients have an increased diagnostic delay as compared to non-Hispanic Caucasian patients, with a lower ALSFRS-R score and vital capacity at the initial clinic visit.”2
Language differences are a considerable barrier for Hispanic or Latino patients in Dr. Karra’s California clinic. “Several of these patients followed up in the ALS clinic but were still unaware or unable to navigate the websites to connect with local ALS organizations and sign up for equipment through loan lockers,” she shares. For those unable to access resources or fully comprehend available options, the path to ALS care is riddled with challenges. This often leads to reduced participation in clinical studies and a limited understanding of experimental therapies that could impact their quality of life.
Addressing the Health Equity Gap Through Innovative Solutions
Dr. Karra has observed that “genetic testing is less frequent in low-resource settings, and there is similarly decreased access to multidisciplinary ALS clinics for these patient populations, a factor that has been previously shown to affect overall disease prognosis.”3 The lack of resources, from genetic testing to transportation for clinic visits, coupled with low health literacy and cultural barriers, often prevents patients from pursuing essential treatments. Dr. Karra points out that “the financial burden of arranging transportation and coming to the clinic during work hours can be an additional prohibitive factor,” illustrating the impact of social determinants of health on ALS care accessibility.
With the urgency of these inequities in mind, Target ALS has launched community-based pop-up clinics designed to provide convenient, one-time blood collections in underserved communities nationwide. Through this initiative, Target ALS aims to address the scarcity of racially and ethnically diverse data on those living with ALS and enable more inclusive research on the genetic and environmental factors affecting ALS progression. As Dr. Karra highlights, “The racial and ethnic diversity of ALS genetic datasets will be paramount for advancing our understanding of disease pathophysiology and driving therapeutic discovery, and increasing the number of diverse participants in clinical trials is critical.”
Ground-Level Initiatives for Inclusive Care
Having witnessed the challenges in her clinic, Dr. Karra developed an innovative pilot project to improve awareness and inclusion for those living with ALS with Spanish as their native language. “After seeing how strongly the language barrier for primarily Spanish-speaking patients affected their access to care and, specifically awareness of clinical studies, I developed a pilot project idea for generating an automatic pop-up message through our electronic health record in the patient’s preferred language, informing patients about ongoing ALS clinical trials at our institution,” she shares. This project represents the small yet impactful steps needed to make ALS research more inclusive, ensuring that information on trials and care resources reaches all patients, regardless of language.
Dr. Karra believes that “direct interactions and conversations with patients and their families” are essential to understanding and addressing the unique challenges faced by people with ALS in underrepresented groups. Moving forward, she emphasizes the need for “creative solutions to bring care to those patients who are unable to shoulder the burden of coming to the clinic.” Dr. Karra advocates for the expansion of tele-neurology and other outreach strategies that can lessen logistical barriers for these populations.
The Role of Social Determinants in ALS Outcomes
Social determinants of health, such as socioeconomic status, education, and language, play a significant role in ALS care and outcomes. “Education access and quality can affect health literacy,” Dr. Karra notes, adding that the complexities of ALS care are compounded by limited digital literacy among ALS patients. These factors often amplify disparities in treatment engagement and retention, especially for elderly and chronically ill patients who may not feel empowered to seek continued care. Dr. Karra states, “We must also promote provider education and training in cultural sensitivity and bias-free care of vulnerable populations,” recognizing that healthcare practitioners play a vital role in bridging these gaps.
Through Target ALS’s pop-up clinics and Dr. Karra’s efforts, an actionable path forward is forming. These initiatives are designed to bring essential resources directly into diverse communities, allowing researchers to collect data representing the full ALS population, not just a narrow segment. This level of inclusivity is essential to building a future where effective ALS therapies are accessible to all, helping patients not only access the care they need but actively participate in shaping it.

As Dr. Karra insightfully puts it, “Ongoing research in this area continues to highlight the importance of understanding the root causes of disparities in healthcare (including access to care) and developing solutions to overcome them.” With these initiatives, Target ALS and its partners are working to create a more equitable healthcare landscape for all those impacted by ALS. For more information on our Pop-Up Clinic Initiative, please email Laura.Dugom@targetals.org.
- Perez MA, Reyes-Esteves S, Mendizabal A. Racial and Ethnic Disparities in Neurological Care in the United States. Semin Neurol. 2024 Apr;44(2):178-192. doi: 10.1055/s-0043-1778639. Epub 2024 Mar 14. PMID: 38485124. ↩︎
- Brand D, Polak M, Glass JD, Fournier CN. Comparison of Phenotypic Characteristics and Prognosis Between Black and White Patients in a Tertiary ALS Clinic. Neurology. 2021 Feb 9;96(6):e840-e844. doi: 10.1212/WNL.0000000000011396. Epub 2020 Dec 28. PMID: 33372030.
Chen S, Carter D, Brockenbrough PB, Cox S, Gwathmey K. Racial disparities in ALS diagnostic delay: a single center’s experience and review of potential contributing factors. Amyotroph Lateral Scler Frontotemporal Degener. 2024 Feb;25(1-2):112-118. doi: 10.1080/21678421.2023.2273361. Epub 2024 Jan 23. PMID: 37909302.
Raymond, J., Nair, T., Gwathmey, K.G. et al. Racial Disparities in the Diagnosis and Prognosis of ALS Patients in the United States. J. Racial and Ethnic Health Disparities(2024). https://doi.org/10.1007/s40615-024-02099-6 ↩︎ - Traynor BJ, Alexander M, Corr B, Frost E, Hardiman O. Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996-2000. J Neurol Neurosurg Psychiatry. 2003 Sep;74(9):1258-61. doi: 10.1136/jnnp.74.9.1258. PMID: 12933930; PMCID: PMC1738639.6. Saadi A, Mendizabal A, Mejia NI. Teleneurology and Health Disparities. Semin Neurol. 2022 Feb;42(1):60-66. doi: 10.1055/s-0041-1742194. Epub 2022 May 16. PMID: 35576930. ↩︎