What is Dementia?
Dementia is the persistent disorder of mental processes marked by difficulties with memory, changes in personality, and impaired reasoning. Dementia is not a specific disease, but rather an all-encompassing term for these cognitive impairments.
The cause of dementia varies and it can affect people differently by causing different symptoms. All patients suffering from dementia have experienced some damage to or loss of nerve cells and their connections in the brain.2
What are the Most Prevalent Types of Dementia?
The different types of dementia are determined by the area of the brain that has nerve damage. The following categorizations of dementia can affect people differently by causing different symptoms. These causes of dementia are often differentiated based on the proteins identified in affected areas of the brain.
Alzheimer’s Disease
Alzheimer’s disease is the most common cause of dementia. This cause of dementia is irreversible and progressive. It slowly destroys memory and cognitive abilities, preventing late-stage patients from carrying out even simple tasks. Alzheimer’s disease is most common in older adults.
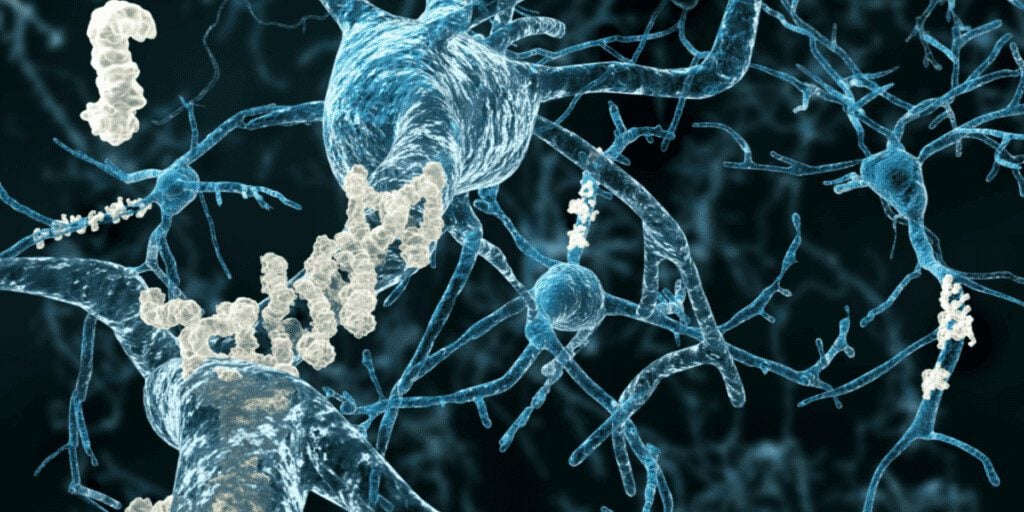
Patients with Alzheimer’s disease have amyloid plaques and neurofibrillary tangles in their brains.
Plaques are abnormal deposits of Beta-amyloid protein that clump together and collect between neurons. Beta-amyloid 42 is one form of the amyloid protein that has been identified in Alzheimer’s patients. It has a high propensity to form amyloid plaques. These plaques are suspected to cause neuron death in the Alzheimer’s brain, although this is still a highly active area of research and the exact mechanism of toxicity is not completely known.
Neurofibrillary tangles are abnormal accumulations of a protein called tau that collect inside neurons. In healthy individuals, tau stabilizes important structures in the cell called microtubules. In those with Alzheimer’s disease, tau sticks to other tau molecules, forming twisted threads that eventually lead to tangles inside neurons. These tangles block the neuron’s ability to transport important cellular cargo effectively along microtubules and hinders communication with other neurons.3
Lewy Body Dementia
Lewy body dementia (LBD) is a disease associated with abnormal deposits of the alpha-synuclein protein. These deposits are called Lewy bodies and affect chemicals in the brain leading to issues with thinking, mood, behavior, and movement.
LBD typically affects patients over the age of 50 and tends to affect men more often than women. It is one of the most common causes of dementia, yet diagnosing LBD can be challenging. This is because early LBD symptoms are often confused with those of other brain diseases and even psychiatric disorders.4
The most common dementia symptoms in LBD patients are visual hallucinations, random changes in attention and wakefulness, disorganized ideas, and severe loss of thinking abilities. The unpredictability of a Lewy body dementia patient’s cognitive functions throughout the day is what sets this disease apart from Alzheimer’s or other forms of dementia.
Vascular Dementia
Vascular dementia is characterized by dementia symptoms caused by conditions that affect the blood vessels in the brain. The size, location, and number of vascular changes can significantly affect brain function and cognition. This form of dementia may occur alone or concurrently with Alzheimer’s disease.
Certain conditions disrupt the flow of blood and oxygen supply in the brain which damages blood vessels. This damage can be identified as abnormalities in MRI scans. Some of the identified causes of vascular dementia include cardiovascular disease, cerebrovascular disease, cerebral hypoperfusion (reduced blood flow), and blood vessel diseases.5
Frontotemporal Dementia
Frontotemporal dementia (FTD) is the result of damage to neurons in both the frontal and temporal lobes of the brain. Symptoms of FTD can include changes in emotion processing, flat affect, difficulty communicating, and issues with motor functions such as walking. FTD is a rare form of dementia, but tends to appear in younger patients than the other types. About 60% of people with FTD are between 45 and 64 years old.6
Symptoms of frontotemporal dementia are progressive, meaning they become worse as time passes. Early-stage patients may only display one symptom, but as the disease progresses and other areas of the brain are affected, other symptoms will appear.
There are three types of frontotemporal disorders, all with some elements of dementia:
1. Behavioral variant frontotemporal dementia (bvFTD)
This is the most common type of FTD. People with bvFTD exhibit changes in personality, behavior, and judgment. These patients may have some problems with cognition, but they generally retain function of their memory.
Patients experiencing bvFTD may have problems thinking through logical steps, difficulty prioritizing tasks, and may act impulsively or say inappropriate things. This last symptom often makes bvFTD difficult to identify because friends and family members of a person behaving in this way may think they are just acting out. The reality is that people with bvFTD are unable to control their behaviors and lack any awareness of their illness.
2. Primary progressive aphasia (PPA)
Aphasia refers to the inability to understand and use language. Those with PPA experience changes in their ability to communicate through speech, reading, writing, and understanding what others are saying.
Those with PPA will first experience language difficulties and later develop problems related to memory, reasoning, and judgment. PPA patients may also develop some drastic behavior changes, similar to those seen in people with bvFTD.
3. FTD movement disorders
There are four neurological movement disorders associated with FTD, both of which are rare and occur only when the parts of the brain that control movement are affected.
Corticobasal syndrome is the progressive loss of the ability to control movement. A person with this syndrome may maintain their normal strength, but become unable to use their hands or arms to perform a movement such as closing a button.
Progressive supranuclear palsy is defined by issues with balance and walking. Palsy refers to paralysis often accompanied by involuntary tremors. Those with progressive supranuclear palsy often move slowly, have unexplained falls, and experience stiffness in the neck and upper body. Trouble with eye movements often define this condition and give affected patients a perpetual stare.
Frontotemporal dementia with parkinsonism involves movement problems like those seen in patients with Parkinson’s disease as well as changes in behavior or language. Parkinson’s-like symptoms include slowed movement, stiffness, and balance problems. This condition may be inherited and caused by a mutation of the tau protein.
Overview of ALS and Dementia
Those with ALS always experience a loss in motor functions from damage to their motor neurons resulting in physical paralysis, but many also experience dementia-like cognitive symptoms. Given the high coincidence of these clinical diagnoses, determining the causes and potential treatment for cognitive impairment in ALS has gained recent attention There is some debate on whether ALS and dementia arise from the same pathological or genetic cause or whether they arise from distinct pathologies, concurrently.
ALS and FTD have shared genetic and pathological etiologies therefore overlap in behavioral or cognitive symptoms may be observed. Mutations in C9orf72, TARDBP, FUS genes, to name a few, can lead to either FTD or ALS or both clinical diagnoses.10 In addition, TDP43 proteinopathy is a neuropathological hallmark found in the majority of ALS cases and in approximately 50% of FTD cases. FTD-ALS is a combination of bvFTD and motor neuron disease. People with both FTD and ALS will experience behavioral changes along with the progressive muscle weakness that defines ALS. Either disease may show symptoms first with symptoms of the other condition developing over time.
Some of the most common FTD symptoms in ALS patients include1:
- Withdrawal/lack of interest in things
- Lack of emotion
- Reduced spontaneity
- Loss of inhibition
- Restlessness or overactivity
- Increased inappropriate social interactions
- Mood swings
- Memory loss
- Loss of speech and/or language comprehensive
- Decrease in ability to problem-solve
How to Diagnose Cognitive Impairment in ALS Patients
Tests for Cognitive Impairment and ALS
Testing for both cognitive impairment, such as dementia, and ALS is not straightforward and there is no single diagnostic test that will confirm either condition. With either condition, a diagnosis should be made earlier rather than later. Early detection of dementia or ALS can provide patients with medical benefits, emotional benefits, and more time to plan for the future. The following are common ways to test for cognitive impairment and ALS.
Brain Scans
Both magnetic resonance imaging (MRI) and computed tomography (CT) scans are used in the diagnosis of certain types of dementia. These types of brain scans may reveal tumors, evidence of strokes, damage from head trauma, or a buildup of fluid in the brain. They could also reveal the plaques and tangles that define Alzheimer’s disease.
In the process of diagnosing ALS in patients with dementia symptoms, MRIs and CT scans can be used to rule out Alzheimer’s or other identifiable forms of dementia. In patients with confirmed ALS, MRI is used to exclude other conditions that may be occurring concurrently.
Other Cognitive and Behavioral Impairment Screening Tools
A neuropsychological evaluation is a way to diagnose cognitive and behavioral impairment in ALS patients. This form of evaluation includes tools that detect behavioral disorders and language impairment.8
Criteria related to the diagnosis of cognitive impairment include evidence of language dysfunction or social issues. Criteria related to assessing behavioral impairment include identifying the presence of apathy and any psychotic symptoms such as delusions.
ALS patients who undergo this evaluation may receive results that indicate the presence of both cognitive and behavioral impairment, one without the other, or ALS without dementia-like symptoms.
Risk Factors of Dementia
The likelihood of developing one of the conditions of dementia is made higher by several identified risk factors. Some risk factors can be prevented, but others cannot and will lead to dementia symptoms.
Here are the risk factors for dementia:
- Age. The risk of developing all types of dementia increases with the advancement of a person’s age.
- Genetics. A family history of dementia may increase the risk of developing certain types of the condition. Researchers have identified genes that increase the risk of developing Alzheimer’s disease in particular.7 Those with Alzheimer’s in their family history are considered to have a greater risk of developing the disease, however, it is not guaranteed that they will.
- Lifestyle choices such as smoking. Smoking has recently been found to increase the risk of cognitive disorders and dementia. This could be due to an increase in vascular diseases in smokers.
- Cholesterol. People with higher levels of “bad” cholesterol may be more predisposed to develop vascular dementia and possibly Alzheimer’s disease.
- Atherosclerosis. Atherosclerosis is the buildup of plaque from fatty substances, cholesterol, and other substances in a person’s arteries.
- Diabetes. Diabetes may increase a person’s likelihood of developing dementia and is also a risk factor for atherosclerosis and stroke. People with diabetes are more likely to develop vascular dementia for those reasons.
- Plasma homocysteine. Homocysteine is a type of amino acid. People with higher-than-average levels of homocysteine in their blood may be more likely to develop dementia.
Are There Treatments for Dementia in ALS?
Unfortunately, there is no cure for dementia in ALS patients.
What are the Next Steps Involved for ALS Patients with Dementia?
ALS patients with dementia should attend regular follow-up visits with their healthcare team in order to track the progression of their condition. It is wise to begin making plans for the future as soon as dementia is identified in ALS patients, as they may become resistant to reasoning and deny their illness as it progresses. Cognitive issues may interfere with treatment decisions, so it is important for ALS patients to have a supportive care team that can step in if assistance is needed.
Support Groups for ALS and Dementia Patients or Caregivers
There are many resources available to ALS patients living with dementia as well as their loved ones. Support groups can help patients and caregivers discuss and overcome the stressors related to a dementia diagnosis.
Support groups can be found in every state. Talk to a local healthcare provider for recommendations about support groups near you.
Tips for Better Routine Management and Care for ALS Dementia Patients
Certain interventions can help people with ALS and dementia cope with the condition. Here are a few tips to manage and care for ALS dementia patients:
- Create a simple daily routine for the patient to follow and help guide them through it each day
- Supervise the ALS patient as they walk and eat to avoid accidents that could be fatal
- Seek physical and speech therapy for patients who can benefit from them early in the progression of their disease
- Use lots of patience when communicating with and supporting the ALS patient. ALS and dementia are two diagnoses that are difficult to accept and those who receive them need extra compassion to help them cope.
Frequently Asked Questions
Does ALS Cause Cognitive Decline in Most Patients?
Recent studies have found that up to half of ALS patients experience cognitive impairment. Researchers are working to understand whether ALS causes cognitive decline or if the two conditions happen concurrently.
Is ALS with Dementia Hereditary?
Certain types of ALS and dementia have family history ties. Familial ALS makes up about 10% of ALS cases and is categorized by more than one person in a family being diagnosed with ALS. Alzheimer’s disease also has evidence of hereditary genes, but a person with Alzheimer’s in their family may not always have the disease themselves.
Is Lewy Body Dementia Related to ALS?
Lewy body dementia is one type of dementia that can be experienced by ALS patients.
Is ALS Inherently Related to Alzheimer’s?
Not all patients diagnosed with ALS will also have Alzheimer’s disease. About 50% of ALS patients will develop some form of dementia. Alzheimer’s disease is the most common dementia diagnosis.
What are Clinical symptoms of FTD in ALS?
People with FTD and ALS exhibit changes in behavior, personality, and language skills and cognitive function. They may also have changes in motor skills such as difficulty walking, trouble with coordination, and issues speaking.
What percent of ALS patients have FTD?
Up to 50% of ALS patients have some form of dementia. ALS patients receive a Frontotemporal dementia (FTD) diagnosis in 5-25% of cases.
SOURCES
1. WebMD. (n.d.). Dementia in amyotrophic lateral sclerosis (Lou Gehrig disease). Retrieved November 6, 2022, from https://www.webmd.com/alzheimers/dementia-amyotrophic-lateral-sclerosis
2. Mayo Foundation for Medical Education and Research. (2022, October 12). Dementia. Mayo Clinic. Retrieved November 6, 2022, from https://www.mayoclinic.org/diseases-conditions/dementia/symptoms-causes/syc-20352013
3. U.S. Department of Health and Human Services. (n.d.). What happens to the brain in alzheimer’s disease? National Institute on Aging. Retrieved November 6, 2022, from https://www.nia.nih.gov/health/what-happens-brain-alzheimers-disease
4. U.S. Department of Health and Human Services. (n.d.). What is lewy body dementia? causes, symptoms, and treatments. National Institute on Aging. Retrieved November 6, 2022, from https://www.nia.nih.gov/health/what-lewy-body-dementia-causes-symptoms-and-treatments
5. U.S. Department of Health and Human Services. (n.d.). Vascular dementia: Causes, symptoms, and treatments. National Institute on Aging. Retrieved November 6, 2022, from https://www.nia.nih.gov/health/vascular-dementia
6. U.S. Department of Health and Human Services. (n.d.). What are frontotemporal disorders? causes, symptoms, and treatment. National Institute on Aging. Retrieved November 6, 2022, from https://www.nia.nih.gov/health/what-are-frontotemporal-disorders
7. Mayo Foundation for Medical Education and Research. (2021, May 6). The role of genes in your alzheimer’s risk. Mayo Clinic. Retrieved November 6, 2022, from https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-genes/art-20046552
8. Susan C Woolley, Beth K Rush, Considerations for Clinical Neuropsychological Evaluation in Amyotrophic Lateral Sclerosis, Archives of Clinical Neuropsychology, Volume 32, Issue 7, November 2017, Pages 906–916, https://doi.org/10.1093/arclin/acx089
9. 10 early signs and symptoms of alzheimer’s. Alzheimer’s Disease and Dementia. (n.d.). Retrieved November 6, 2022, from https://www.alz.org/alzheimers-dementia/10_signs
10. Abramzon YA, Fratta P, Traynor BJ and Chia R (2020) The Overlapping Genetics of Amyotrophic Lateral Sclerosis and Frontotemporal Dementia. Front. Neurosci. 14:42. doi: 10.3389/fnins.2020.00042





